Northern Illinois Retina has been providing comprehensive retinal care since 1991. As the only full-time, full-service retinal provider in the northern Illinois area, you can be assured that we are always available and will provide you with the most updated state of the art retinal care.
Diagnostic Studies We Perform Include:
OCT
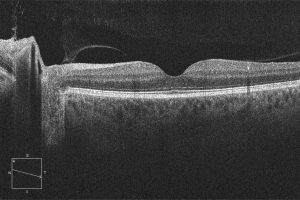 Optical Coherence Tomography is a non-invasive imaging test. OCT uses light waves to take cross-sectional pictures of your retina. With OCT, your ophthalmologist can see each of the retina’s distinctive layers. This allows your ophthalmologist to map and measure retinal thickness.
Optical Coherence Tomography is a non-invasive imaging test. OCT uses light waves to take cross-sectional pictures of your retina. With OCT, your ophthalmologist can see each of the retina’s distinctive layers. This allows your ophthalmologist to map and measure retinal thickness.
OCT A
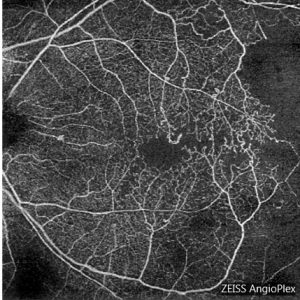 Fluorescein Angiography Optical Coherence Tomography Angiography is a new, non-invasive imaging system that generates volumetric data of retinal and choroidal layers. It has the ability to show both structural and blood flow information in the retina.
Fluorescein Angiography Optical Coherence Tomography Angiography is a new, non-invasive imaging system that generates volumetric data of retinal and choroidal layers. It has the ability to show both structural and blood flow information in the retina.
Fluorescein Angiography
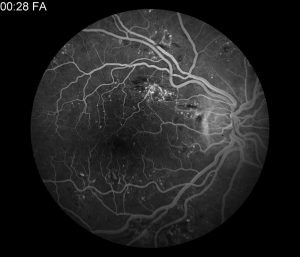 Fluorescein Angiography Fluorescein angiography is a diagnostic procedure that uses a special camera to photograph the light-sensitive retina and more specifically, the blood vessels in the back of the eye.
Fluorescein Angiography Fluorescein angiography is a diagnostic procedure that uses a special camera to photograph the light-sensitive retina and more specifically, the blood vessels in the back of the eye.
First, fluorescein, a water-soluble dye, is injected into a vein in the arm. The dye travels throughout the body, and as it passes through the blood vessels of the retina, a special camera flashes a blue light into the eye and takes multiple photographs.
If the blood vessels are abnormal, the dye may leak into the retina or stain the blood vessels. Damage to the lining underneath the retina or the appearance of abnormal new blood vessels growing beneath or on the surface of the retina may also be revealed.
Fluorescein angiography is useful in detecting several diseases of the retina. Diabetes, the leading cause of blindness in patients UNDER the age of 65, can cause the blood vessels of the retina to leak fluid or blood and can cause new blood vessels to grow on the retinal surface.
Age-related macular degeneration is the leading cause of blindness in patients OVER the age of 65, and it can also be detected with and monitored by fluorescein angiography.
Most important for your ophthalmologist and surgeon, fluorescein angiography provides a picture of exactly where the retinal blood vessels are leaking and can thus guide laser treatment with pinpoint accuracy, as well as monitoring response to treatment.
Visual Field
A Goldmann visual field test is an eye examination that can detect dysfunction in central and peripheral vision which may be caused by various medical conditions such as glaucoma, stroke, pituitary disease, brain tumors, or other neurological deficits. Visual field testing can be performed clinically by keeping the subject’s gaze fixed while presenting objects at various places within their visual field.
In-Office Retinal Procedures We Perform Include:
Cryotherapy
With cryotherapy, an extremely cold probe is applied to the outside of the eye, or sclera. The sclera transmits the cold inward so the freezing temperature is effectively applied to the retina.
Similar to a laser’s heat, the intense cold stimulation of the retina can seal abnormal leaky retinal blood vessels or retinal tears by stimulating a biologic pigment seal.
Surgeons often prefer using cryotherapy over laser treatment when problems arise with the far outside corners of the retina, especially when the patient has a vitreous hemorrhage or cataract obscure the passage of light into the eye, limiting the effectiveness of a laser.
Cryotherapy is often performed in conjunction with surgical treatments for retinal detachment, such as pneumatic retinopexy or scleral buckle surgery.
Usually, patients often require local anesthesia before the cryotherapy and eye drops and an eyepatch following surgery.
Laser
Laser, or “hot” treatment to the retina, uses different wavelengths of light to seal leaking blood vessels (diabetes or wet macular degeneration) or to induce a biologic pigment seal around retinal tears that can be visualized through a special lens applied to the eye.
Pneumatic Retinopexy
Pneumatic retinopexy is an in-office procedure that can be performed to correct selected retinal detachments.
Pneumatic retinopexy is performed under local anesthesia in our office as an outpatient procedure.
An alternative to scleral buckling surgery, which is performed in an operating room, pneumatic retinopexy requires no hospitalization, general anesthesia, or cutting of the eye.
Pneumatic retinopexy is effective only for superior retinal detachments and tears.
The retinal tear is sealed with cryotherapy. Using a needle, the surgeon then injects a gas bubble inside the vitreous cavity of the eye. (Hence the term pneumatic.)
It is crucial for the success of the procedure that the patient maintains a specific position of their head (for several days up to a week) as instructed by their surgeon so that the retinal tear can be effectively sealed by the gas bubble pushing on the retina inside the eye.
The gas bubble in the vitreous cavity of the eye expands for several days and takes two to six weeks to disappear completely.
During this time, the patient must AVOID AIRPLANE TRAVEL OR TRAVEL TO HIGH ALTITUDES. High altitudes can cause the gas bubble to expand, increasing the pressure within the eye, which can lead to severe eye damage.
THE PATIENT MUST ALSO TAKE CARE NOT TO LIE IN THE FACE-UP (SUPINE) POSITION. If the gas bubble were to rest against the lens of the eye, a cataract or high pressure within the eye may form. Your surgeon may instruct you to use antibiotic eye drops following the surgery.
Retinal detachments that are not amenable to treatment with pneumatic retinopexy (inferior retinal detachments, or older detachments with scar tissue) are usually treated in the operating room with a scleral buckle or pars plana vitrectomy.
Anti-VEGF Treatment for Wet Age-Related Macular Degeneration
Anti-VEGF treatment is a way to slow vision loss in people who have a condition known as “wet” age-related macular degeneration (AMD).
AMD is the leading cause of vision loss in people 65 years or older in the United States.
You rely on your macula whenever you read, drive, or do other activities that require you to focus on precise details. A person with AMD loses the ability to perceive fine details both up close and at a distance. This vision loss usually affects only your central vision.
There are two types of AMD. About 90% of people with AMD have the atrophic or “dry” form of AMD, which develops when the tissues of the macula grow thin with age. About 10% develop the exudative or “wet” form of AMD.
With wet AMD, abnormal blood vessels grow underneath the retina. These unhealthy vessels leak blood and fluid, which can scar the macula. Vision loss can be rapid and severe.
Researchers have found that a chemical called vascular endothelial growth factor, or VEGF, is critical in causing abnormal blood vessels to grow under the retina. Scientists have developed several new drugs that can block the trouble-causing VEGF.
These are referred to as “anti-VEGF” drugs, and they help block abnormal blood vessels, slow their leakage, and help reduce vision loss.
Treatment with the anti-VEGF drug is usually performed by injecting the medicine with a very fine needle into the inside of your eye. Your surgeon will clean your eye to prevent infection and will administer an anesthetic into your eye to reduce pain during the injection.
Usually, patients receive multiple anti-VEGF injections over the course of many months. There is a small risk of complication with anti-VEGF treatment, usually resulting from the injection itself (possibility of inducing infection during the injection.) However, the benefits of this treatment greatly outweigh the small risk of complications.
Anti-VEGF medications are a step forward in the treatment of wet AMD because they target the underlying cause of abnormal blood vessel growth.
We use all three currently available anti-VEGF medications: Avastin (Bevacizumab), Lucentis – 0.3 & 0.5 (Ranibizumab), Eylea (Afibercept).
This treatment offers new hope to those affected with wet AMD. Although not every patient benefits from anti-VEGF treatment, a large majority of patients achieve the stabilized vision, and a significant percentage can improve to some degree.
Other diseases often treated with Anti-VEGF injections:
- Diabetic Retinopathy
- Venous Occlusions (BRVO, CRVO)
Photodynamic Therapy for Age-Related Macular Degeneration / Central Serous Retinopathy
Age-related macular degeneration (AMD) is a deterioration or breakdown of the macula. The macula is a small area at the center of the retina in the back of the eye that allows us to see fine details clearly and perform activities such as reading and driving.
In exudative or “wet” AMD, abnormal blood vessels can grow in a layer beneath the retina, leaking fluid and blood and creating distortion or a large blind spot in the center of your vision.
Photodynamic therapy (PDT) – an outpatient procedure involving the use of a special light-activated drug (visudyne)– is used to treat some patients with wet AMD and also patients with another macular leakage syndrome central serous retinopathy (CSR.) A laser tuned to a specific wave length then activates the drug which seals the leaking vessels.
With PDT, the inactive form of the drug is usually injected into a vein in the arm, where it travels to and accumulates in abnormal blood vessels under the center of the macula.

